Overview
Venous thromboembolism, including deep vein thrombosis and pulmonary embolism, imposes a major burden on the US healthcare system. The disorder is estimated to cost more than $5 billion annually, an average of $20,000 per treated patient per year. Venous thromboembolism risk is associated with about 8 million hospitalized non-surgical patients per year in the US, causing 900,000 blood clots per year and leading to 100,000 deaths.
Intermountain Healthcare’s insurance plan, SelectHealth, covers more than 1 million people, and in this population, the frequency of pulmonary embolism is greater than 65 per 100,000 persons. This estimates approximately 650 possible patient encounters of this diagnosis per year.
Traditional risk-scoring models focus on diagnostic decision-making and treatment guidelines that lack specificity around risk stratification that uses important biomarkers and imaging data. The main surrogate for more aggressive treatment is controlling blood pressure. But there is unclear direction on how to incorporate brain natriuretic peptide lab values, troponin lab values, and right heart ventricle–to–left heart ventricle ratios in treatment. To understand the severity of a patient’s disease and the probability of adverse outcomes, clinicians must address variation in treatment and then suggest investment opportunities for point-of-care solutions that can be implemented at patient admission.
Challenges
Intermountain needed to be able to access and properly review their data to determine risk stratification and treatment options for patients with pulmonary embolism. The team required a tool that would analyze the levels of clinical biomarkers in patients with pulmonary embolism, provide information about the mortality rates for these patients, and generate insights into how different treatment options affect outcomes for pulmonary embolism.
KEY QUESTIONS
-
What is the current standard of care for pulmonary embolism across our health system in rate of bleed, 30-day mortality, and 30-day readmission?
-
What are traditional and novel biomarkers of interest in stratifying severity and risk of patients?
-
What is the cost variation in selected treatment approaches of patients with pulmonary embolism?
-
How do we sub-segment patients into risk categories to define programmatic directives suggestive to treatment path?
Results to Date
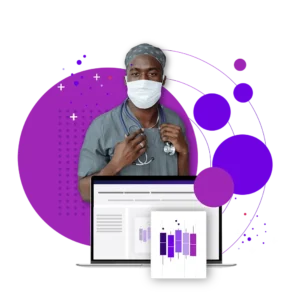
The team at Intermountain performed an analysis of standard of care compared with national benchmarks in outcomes regarding pulmonary embolism response for its tertiary care centers. The care team based evaluated outcomes based on current literature as well as variability in cost of episode of care by facility and treatment path. This opened visibility to a state of care that had never previously been realized with data at Intermountain.
The team’s markers of interest included brain natriuretic peptide lab values, troponin lab values, and right ventricle–to–left ventricle ratios (derived from MDClone’s NLP Studio). The team first performed a retrospective analysis of cost variation by selected treatment approaches. They then used the pulmonary embolism severity index (PESI) score and classification for patients on admission — as well as other clinical markers of interest — to build a care process model for treatment approaches based on severity and risk stratification.
The estimated claim cost for short-term pulmonary embolism is $7,605, compared with long-term treatment, which is estimated to be $48,751 per patient. Hospitalizations account for 84% of total annual pulmonary embolism health costs. Intermountain discovered the following potential benefits of implementing a risk model for patients with pulmonary embolism:
-
Leveraging the MDClone self-service data platform to develop a pre-discharge model for venous thromboembolism treatment could avert approximately 1,180 venous thromboembolism events annually across Intermountain.
-
The delta cost savings of early detection and proactive treatment, as opposed to long-term care, could represent a total savings opportunity of greater than $24 million.
-
With the targeted pulmonary embolism cohort risk model implemented, the estimated per member per month savings from reduced hospitalizations could reach a total of greater than $1 million annually.
-
With the support of better risk stratification on patient presentation, patients can experience a more streamlined approach to treatment based on severity.
-
The ability to set a care process in place for the minimum metrics needed for addressing severity of pulmonary embolism and to triage care based on biomarkers of interest.
INSIGHTS
Right heart ventricle–to–left heart ventricle ratio is not always a strong indicator when employing computed tomography, and ultrasound is a better modality for this. Brain natriuretic peptide and troponin should be drawn as soon as diagnosis occurs to assess risk. PESI plus brain natriuretic peptide, right heart ventricle–to–left heart ventricle ratio, and troponin is a great milieu of biomarkers for the stratification and prediction of outcome.
In subsequent retrospective analysis, using the PESI score with brain natriuretic peptide, right heart ventricle–to–left heart ventricle ratio from MDClone NLP Studio, and troponin values included in a predictive model, there was a strong statistical significance between the rate of bleeding and 30-day mortality. This represents a risk reduction for patients treated with anticoagulation medications only and avoids unnecessary admission for lower-risk categories. Based on the insights gained from the ADAMS Platform, the team determined that physicians at Intermountain need to:
-
Make faster decisions to move higher-risk patients to interventional radiology suites
-
Consider a new lysis therapy or thrombectomy in moderate to high categories
-
Consider thrombectomy in the very high-risk category
Conclusion
Although this use case originated with clinicians at Intermountain’s McKay Dee hospital in Ogden, UT, the insight will lead to a standardized care process model for all patient locations. It also leads to a request for capital funding for a point-of-care solution to use this risk stratification for patients on admission, a quality improvement approach to continuously evaluate thrombectomy and new lysis procedure outcomes, and an abstract for submission to a journal.
“Our work informed how I approach care, and I was able to make a data-informed decision about treatment of a patient last week. The procedure was successful, and the patient was walking around the next day. All of our facilities should adopt this.”